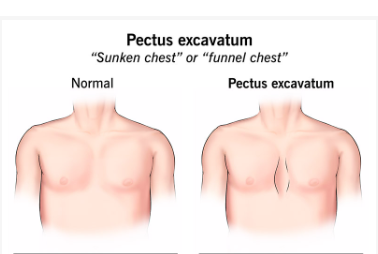
Pectus excavatum frequently appears subtly, as a slow-forming indentation that gradually develops over the early adolescent years. It is rarely visible from the acute self-awareness of adolescence, but it can occasionally be concealed under T-shirts and hoodies. This congenital deformity, which is caused by an abnormal inward development of the sternum, alters a person’s physical function and feelings about it in addition to how they look. Although the disease is statistically more common in teenagers, especially boys, girls and non-binary people who are navigating body image at a sensitive developmental time may also bear the psychological burden.
It goes beyond appearances. The heart and lungs may compress as a result of the sternum pressing inward, decreasing breathing capacity and cardiovascular efficiency. Patients frequently complain of obvious exhaustion, shortness of breath, and reduced stamina. Some people are shocked to discover that their pounding heart and erratic rhythms are caused by a chest wall pressing directly against their heart, not just anxiety.
Pectus Excavatum Surgery – Key Facts
| Category | Details |
|---|---|
| Condition | Pectus Excavatum (Funnel Chest, Sunken Chest) |
| Cause | Congenital defect; sometimes linked to Marfan or Ehlers-Danlos syndromes |
| Visible Sign | Breastbone grows inward, creating a concave or “sunken” appearance of the chest |
| Common Onset | Early teenage years |
| Common Symptoms | Breathlessness, fatigue, irregular heartbeat, depression, poor body image |
| Surgical Treatments | Nuss Procedure (minimally invasive) and Ravitch Procedure (open surgery) |
| Recovery Innovations | Use of cryoablation for pain control, shorter recovery, less need for opioids |
| Ideal Surgery Age | 10–14 years, while chest wall is still flexible |
| Long-term Complications | Rare – may include infection, bar movement, collapsed lung, or recurrence |
| Official Medical Resource |
Previously viewed as cosmetic, surgery is now recognized by experts as a valid medical procedure. Notably, the Nuss procedure’s high success rate and minimally invasive nature have made it the preferred option. Through tiny side incisions, a curved metal rod is slipped behind the sternum during this procedure. The indentation is essentially reversed when the bar is switched, raising the chest wall outward. The bar, which is kept in place for two to three years, subtly changes the patient’s emotional posture in addition to the bone structure.
A more conventional method, the Ravitch treatment is preferred when direct manipulation of the sternum’s stiffness is necessary. Stabilizing plates or a smaller bar are used by surgeons to maintain the bone in its proper position after they remove the excessive cartilage. Both techniques seek to restore critical function as well as symmetry, allowing for deeper breathing and lessening heart compression.
The breakthrough in pain control made possible by cryoablation is what makes contemporary treatment so remarkably effective. It significantly lessens post-operative pain by freezing the nerves between the ribcage. In the past, students had to recover for weeks and faced the possibility of developing an opiate dependent. Many now leave the hospital in a day or two and go back to school far sooner than was previously feasible because of cryoablation and increased surgical precision.
Not only is this a breakthrough in surgery, but it also redefines what is feasible for young people who are torn between social expectations and physical limitations. American Olympic swimmer Cody Miller has publicly talked about using pectus excavatum in competition. He overcame physical constraints to earn medals in Rio despite having a diminished lung capacity. Many young athletes report far better endurance following surgery, which not only relieves physical pain but also gives them a new feeling of self.
Others may have an equally significant emotional shift. Adolescents who have sunken chests frequently experience extreme shame, particularly in social situations and locker rooms. There are remarkably similar stories from all cultures and nations about teenagers avoiding gym class, swimming pools, and even summer vacations due to the guilt they feel about their bodies. Patients report a change in their mental and physical posture following surgery. Shoulders erect. The smiles come back. It gets simpler to make eye contact.
Many people were unable to get the procedure since insurance policies used to classify it as elective or cosmetic. Now, that is changing. Since there is more proof that pectus excavatum causes functional impairments, several providers have begun to grant coverage. This change represents a step toward more equitable access to healthcare and is especially helpful for families that cannot afford to pay out-of-pocket.
However, there are hazards associated with surgery. Although they are uncommon, complications like infection, fluid accumulation, bar displacement, or recurrence following bar removal do occur. Choosing a skilled thoracic surgical team is so essential. Pectus excavatum repair centers are recommended to families because of their significantly greater success rates and better post-operative care.
Social media has also unexpectedly contributed to the narrative’s transformation during the last ten years. Teens who used to keep quiet about their illness now post about their surgery experiences on YouTube and TikTok. Videos of bar removals, post-operative updates, and chest makeovers are encouraging more patients to get treatment sooner. A silent revolution is taking place, in which vulnerability leads to action and visibility leads to vulnerability.
Pectus excavatum surgery is a component of a broader trend in reconstructive and thoracic therapy. The emphasis now encompasses overall well-being rather than just survival or structural repair. To promote a comprehensive rehabilitation, medical teams are increasingly collaborating with psychologists, physical therapists, and dietitians. This integrative method is very novel and illustrates how medicine is changing to accommodate the complex requirements of younger patients.
Even society is changing. Nowadays, discussions about surgical correction are part of body positivity—not as vanity, but as agency. Adolescents are being urged to take early action to protect their health. Parents are paying closer attention. In their evaluations, healthcare professionals are becoming more inclusive and considering emotional as well as functional constraints.
For patients who have surgery, the prognosis is especially promising. Most resume their normal activities in a matter of weeks. In a matter of months, full sports engagement is usually returned. And for a lot of people, the scars represent development rather than flaws.




