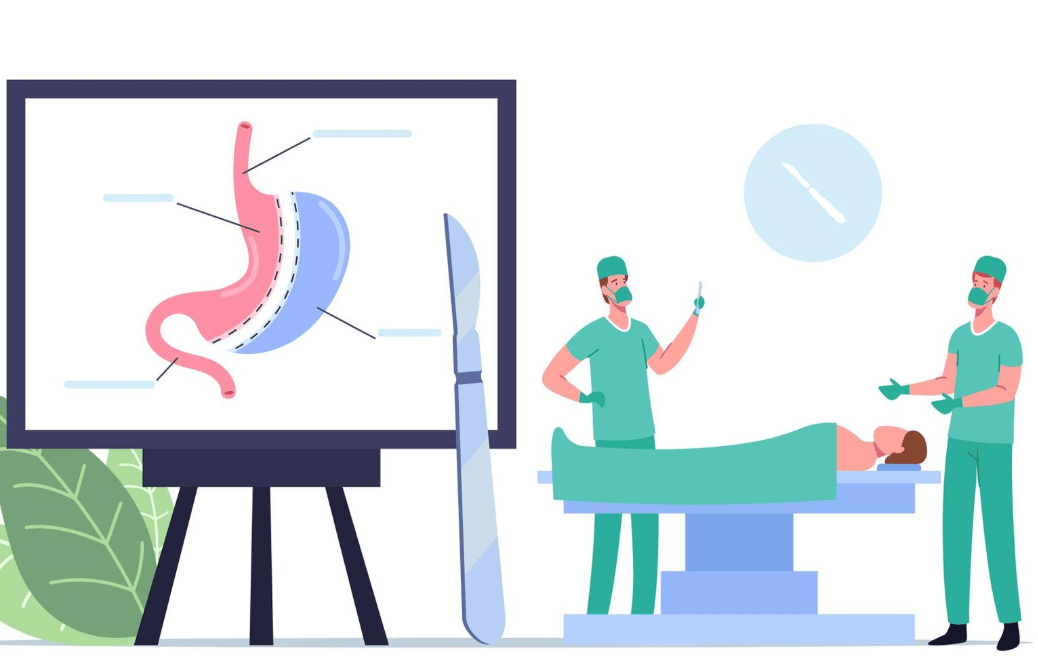
Gastric sleeve surgery has shown itself to be a remarkably effective reset when contrasted with endless diets and short-term solutions. About 80% of the stomach is removed during the procedure, leaving behind a thin, banana-like sleeve. Physical and hormonal barriers to overeating are greatly diminished as a result of this streamlined stomach’s drastic reduction in food capacity and reduction in the hunger hormone ghrelin.
In the last ten years, gastric sleeve surgery has quickly risen to the top of the bariatric surgery market in the US. Surprisingly, only 1% of qualified candidates actually have the operation, despite the fact that over 150,000 procedures are carried out nationwide each year. This disparity reflects the stigma associated with weight loss surgery, which is gradually starting to change as more public figures and celebrities discreetly share their own surgical experiences.
Gastric Sleeve Surgery: Essential Information Table
| Procedure Type | Bariatric (Weight Loss) Surgery |
|---|---|
| Medical Name | Sleeve Gastrectomy |
| Purpose | Reduce stomach size by ~80% to limit food intake |
| Stomach Shape After | Narrow tube, similar to a banana |
| Surgical Method | Minimally invasive (laparoscopic or robotic) |
| Ideal Candidates | BMI ≥ 40, or BMI ≥ 35 with obesity-related illnesses |
| Key Health Benefits | Reduced appetite, fewer hunger hormones, weight loss |
| Conditions It Helps Treat | Type 2 diabetes, hypertension, sleep apnea, joint pain |
| Annual US Procedures | Approximately 150,000 |
| Hospital Stay | Typically 1 to 2 days |
| Post-Op Supplements | Multivitamins, B12, calcium, vitamin D |
| Source | Cleveland Clinic – www.clevelandclinic.org |
Two well-known individuals who underwent surgery for survival rather than vanity after years of public scrutiny and health issues are Rosie O’Donnell and Randy Jackson. Though extremely personal, their changes are similar to those of thousands of people who deal with severe comorbidities like sleep apnea, high blood pressure, and Type 2 diabetes—disorders that gastric sleeve surgery can significantly improve or even cure.
The procedure addresses the mental and physical cycles of overeating by concurrently decreasing stomach size and hormone hunger signals. This approach offers hope without taking any short cuts, which is especially helpful for people who have repeatedly failed with traditional diets. It’s not magic; rather, it’s the combination of human resiliency and medical science, made possible by precise surgery.
Candidates have to go through a number of checkpoints before they reach the operating room. These consist of supervised diet trials, mental health assessments, and occasionally a liquid diet prior to the procedure. The goal is to prepare the body and mind for the ensuing permanent lifestyle changes, not to create obstacles. Dietitians and surgeons collaborate closely with patients to guarantee preparedness and reasonable expectations. Just as important as the actual surgery is this pre-operative period.
The procedure is extremely effective and is usually carried out with laparoscopic instruments through tiny incisions. The majority of patients notice changes in their appetite within two days of returning home. Starting with clear liquids, the post-operative diet gradually progresses to purées, soft foods, and finally small solid meals. The timing of each step is carefully planned to promote healing and retrain the stomach.
After the procedure, it is impossible to compromise on nutritional vigilance. The risk of vitamin and mineral deficiencies increases with decreased stomach capacity. Vitamin B12, calcium, vitamin D, and multivitamins are among the supplements that patients must take. Regular bloodwork monitoring helps identify any imbalances early. The surgery frequently pays for itself in fewer hospital stays and medication requirements, making it surprisingly inexpensive when long-term healthcare savings are taken into account.
Many patients report a change in their relationship with food in addition to physical changes. Meals stop being spontaneous and start to have a purpose. “You learn to steer more carefully, plan each move, and appreciate every mile,” said one former patient, likening her post-surgery mindset to operating a smaller vehicle. The psychological retooling that comes with anatomical changes is encapsulated in this metaphor.
The wider advantages of gastric sleeve surgery are becoming more widely acknowledged by medical professionals in both private clinics and the NHS. It is now considered an essential component of preventive care rather than just a last resort. Following the implementation of structured bariatric programs, clinics in regions with high obesity rates have reported noticeably fewer hospital admissions for complications related to diabetes.
Many surgical centers are now developing integrated weight loss ecosystems through strategic partnerships with fitness professionals, psychologists, and nutritionists. These interdisciplinary teams offer a pathway as well as a process. This strategy is especially novel and gaining popularity around the world, particularly in areas where obesity rates are on the rise.
A silent revolution is occurring in society. Once taboo, conversations about bariatric surgery are now being accepted in the media and among celebrities, albeit cautiously. Even though not every change makes the news, the impact is indisputable. More people are coming forward to ask for assistance after being motivated by those with public platforms. The cultural change has been incredibly successful in raising awareness and lowering stigma.
Preventive surgeries like the gastric sleeve provide a stabilizing influence in post-pandemic healthcare, where rising mental health issues and delayed treatments have put tremendous strain on medical infrastructure. Patients who previously required frequent visits to manage their metabolic syndrome are now doing well with little help. In addition to improving personal health, this development drastically lowers public healthcare costs.
Notwithstanding the favorable results, it’s critical to acknowledge the level of dedication required for gastric sleeve surgery. Discipline, encouragement, and consistent follow-up are necessary for the journey. Although it’s not a quick fix, it’s a lifeline for many people because it realigns behavior and body.
With the advent of personalized medicine and proactive care, gastric sleeve surgery is becoming more and more popular and successful. As a reliable medical intervention, not as a fad. It is a daring and life-changing step toward a longer, healthier life for many who have battled in silence.