Topical corticosteroids were heralded as “miracle creams” when they initially appeared in dermatology. In the present, we are starting to uncover an uncomfortable truth: these same drugs can cause Topical Steroid Withdrawal Syndrome, a very painful rebound condition that some users experience. This disorder, which is frequently concealed by other diagnoses, is coming to light more and more, especially as more patients open up about their struggles on the internet.
A person is typically months or years into using topical steroids by the time they suspect they are suffering from TSW. These creams, which were initially prescribed to treat eczema, contact dermatitis, or even cosmetic lightening, provide temporary relief but have the potential to subtly foster long-term dependence. The arc that patients describe is uncannily consistent: the flare spreads, the steroid stops working, and then they are faced with a new type of pain.
| Key Aspect | Details |
|---|---|
| Condition Name | Topical Steroid Withdrawal Syndrome (TSWS) |
| Alternative Names | Red Skin Syndrome (RSS), Topical Steroid Addiction (TSA) |
| Primary Cause | Prolonged or inappropriate use of topical corticosteroids |
| Typical Symptoms | Redness, itching, burning, flaking, swelling, and insomnia |
| Treatment Options | Stopping steroids, antihistamines, tacrolimus, dupilumab, light therapy |
| Prevention Strategy | Avoid long-term use (over 2 weeks) of topical steroids |
| Common Triggers | Overuse of steroid creams, improper cosmetic use, secondary contact |
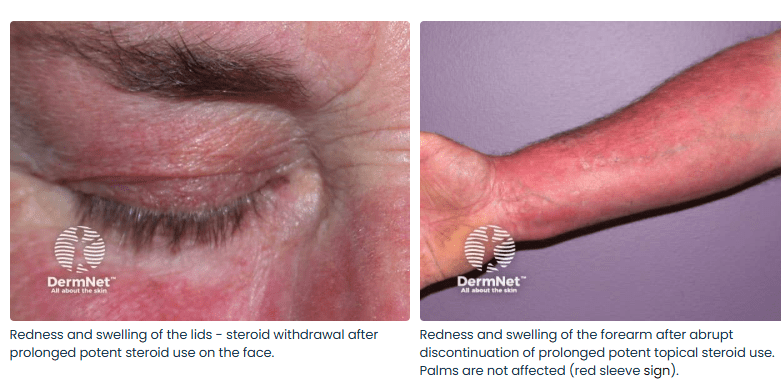
| Diagnosis Signs | “Red sleeve,” “headlight sign,” “elephant wrinkles” |
| Potential Complications | Skin infections, psychological stress, physical immobility |
| Associated Demographic | Children and adults; common among eczema patients |
| Recovery Period | Several months to multiple years depending on severity |
| Risk Factor | Unpredictable individual sensitivity |
| Notable Support Group | ITSAN (International Topical Steroid Awareness Network) |
| Reference Website |
Some people who have Red Skin Syndrome describe their skin as being painted in bright, unpolished colors. The itching gets unbearable. Suddenly, burning sensations flare up. The skin’s surface oozes and flakes. The symptoms are resistant to standard treatments and are frequently misdiagnosed as an acute allergy or worsening eczema. The severity and scope of these reactions following cessation of steroid use are what set TSW apart. These are more than just rashes; they are complete skin barrier shutdowns, which can leave patients bedridden for weeks at a time.
Social media has acted as an accelerant in recent years, raising awareness in areas where traditional medical channels have been quiet. Although they haven’t specifically mentioned TSW, celebrities like Kourtney Kardashian and Cara Delevingne have sparked interest in the topic by posting about inflammatory skin conditions. Many fans start making comparisons and start doubting the creams they have relied on for decades. A common narrative is being shaped by the anecdotal rise of influencer skin journeys: even if something is doctor-approved, exercise caution when applying it.
Corticosteroids were never intended for long-term use, but they were remarkably effective in brief doses. But during prescription, that warning isn’t always highlighted. It’s incredibly simple to get caught up in a cycle of use, flare, reapplication, and further skin damage, particularly in areas where over-the-counter access is still poorly regulated. The onset of TSW symptoms increases the guilt experienced by parents of children with eczema. They had frequently been using the cream in the hopes of getting better.
The syndrome is frighteningly complicated. It causes significant psychological distress in addition to physical discomfort. Patients describe feelings of loneliness, anxiety, and insomnia. In support groups, people talk about the humiliation of public outbursts, the excruciating pain of taking a shower, and the ongoing fear that recovery may never materialize.
There is still division among medical professionals. While some believe TSW is overblown or uncommon, others recognize it as an iatrogenic (doctor-induced) condition. The International Topical Steroid Awareness Network, or ITSAN, has played a key role in bringing people together. Their data-driven advocacy gives victims structure and solace while outlining a more obvious course of action. However, dermatologists’ consensus is still developing—painfully slowly for those who are experiencing these symptoms.
In Japan, where dermatologists believe that up to 12% of adult eczema patients may actually be displaying TSW symptoms rather than uncontrolled dermatitis, a particularly creative approach to treatment has surfaced. While some physicians use non-steroidal topicals like tacrolimus or clindamycin, others are cautiously investigating immune-targeting biologics like dupilumab (Dupixent). Additionally, light therapy has demonstrated promise, particularly in reducing inflammation without the use of novel chemical irritants.
The increase in skin-conscious culture over the last ten years has fueled this discussion. Customers want brands to be transparent. They want an explanation of ingredient lists. They anticipate long-term research to support dermatological claims. Most significantly, they are beginning to question the notion that better skin always results from using more product.
Experts are calling for a significant rethink by emphasizing prevention: no topical steroid should be used for more than two weeks without a reevaluation. Furthermore, secondary exposure is being brought to light by the ripple effect. Since even indirect exposure can cause adult skin to become sensitized, parents who use steroid creams on their children are now advised to wash their hands thoroughly afterward. In limiting the severity of this condition, it is a minor but crucial step.
Medical researchers are getting access to data that would have otherwise been hidden in private diaries thanks to strategic alliances with advocacy organizations and online communities. Narratives are being verified. We are observing patterns. Although slow, recovery is becoming more apparent.