Despite its amazing capacity to restore comfort and dignity, hemorrhoidectomy surgery is rarely discussed publicly but is frequently discussed in whispers. The majority of hemorrhoids are invisible or go away on their own, but a tiny percentage worsen into an excruciating, persistent condition. Surgery provides that group with release as well as relief. Swollen veins in the rectal region cause ongoing discomfort, much like a defective cushion that is continuously adjusted under pressure. Additionally, the option to surgically remove the problem becomes very alluring when topical treatments and home remedies turn into a never-ending cycle of false hope.
Patients, from retired athletes to busy executives, have started to embrace this procedure with cautious optimism in recent years. They frequently come to this conclusion after going through the tiresome cycle of recurrent thrombosis or prolapse, where each episode is more frustrating than the last. There have been quiet but regular reports of celebrities and public figures casually mentioning “a minor surgery that changed everything” on health forums and in podcast interviews. Those in the know instantly recognize the reference, even though it is rarely stated explicitly.
Essential Information on Haemorrhoidectomy Surgery
| Topic | Details |
|---|---|
| Procedure Name | Haemorrhoidectomy |
| Purpose | Surgical removal of problematic hemorrhoids |
| Conditions Treated | Prolapse, thrombosis, strangulation, recurrent hemorrhoids |
| Procedure Types | Excision, stapled, or de-arterialisation (THD) |
| Anesthesia | General anesthesia used in most cases |
| Average Recovery Time | 2 to 8 weeks |
| Common Side Effects | Post-op pain, bleeding during bowel movements, fatigue |
| Estimated Success Rate | Approximately 95% |
| Surgery Frequency | Less than 10% of hemorrhoid patients require this procedure |
| Trusted Medical Source |
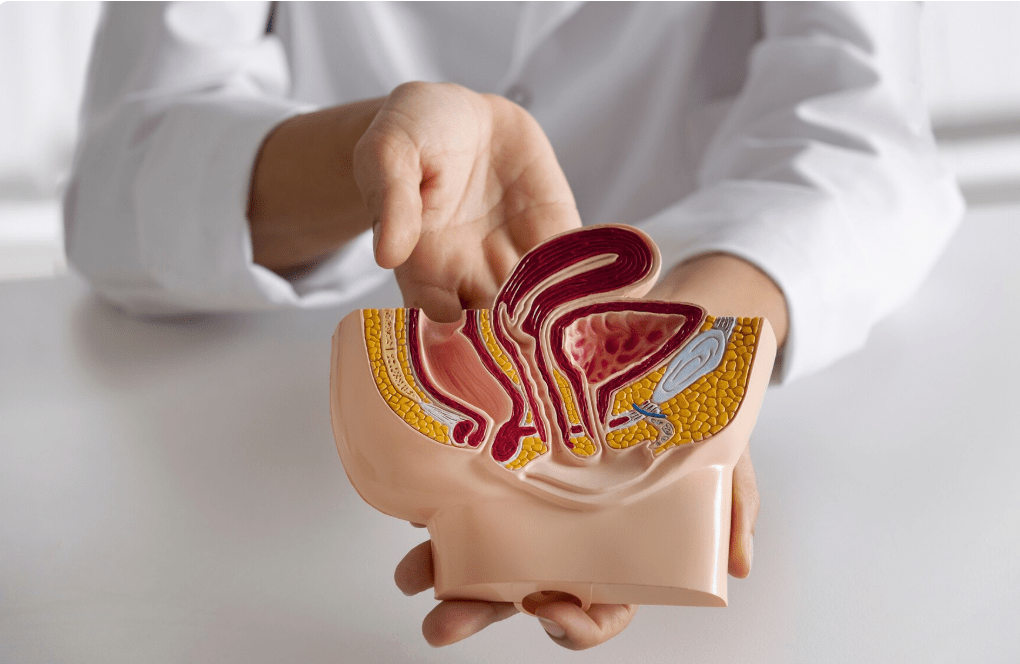
When symptoms just won’t go away, a hemorrhoidectomy is usually the first step. At first, symptoms like a prolapsed bulge, visible swelling, or pain during bowel movements might seem manageable. However, the conversation swiftly moves from conservative treatment to surgical intervention as symptoms worsen from Grade II to Grade IV, which occurs when hemorrhoids become strangled or refuse to retract. The choice is frequently well-considered rather than dramatic. The illness subtly undermines confidence and concentration, especially for professionals who spend a lot of time sitting down. It is not feasible to continue going through such a private ordeal indefinitely.
Prolapse, in which tissue slides out and is difficult to reposition manually, and thrombosis, in which blood clots form inside hemorrhoids, causing excruciating pain and bluish discoloration, are the most frequent complications that lead to hemorrhoidectomy. Stangulation, which occurs when prolapsed tissue becomes trapped and stops receiving blood, is even more serious. In order to avoid tissue death, this kind of emergency necessitates immediate surgical removal. In these cases, the surgery becomes not only beneficial but also necessary.
Under general anesthesia, patients are gently put to sleep during the actual procedure. The surgical technique used will determine whether the hemorrhoids are excised directly, stapled into place, or treated with a more sophisticated procedure called transanal hemorrhoidal de-arterialization (THD). The last strategy is especially novel; it entails identifying and cutting off the arteries supplying the hemorrhoids in order to promote their gradual shrinkage. While the goal of all approaches is to eradicate the symptoms, THD is notable for its smoother recovery curve and less invasiveness.
Following surgery, there is usually a sigh of relief at the start of recovery, followed by a few difficult days. It is normal to experience pain, particularly during the first few bowel movements. However, many patients find that they have shed not only discomfort but also a persistent cloud of anxiety as they gradually return to their regular routines. They talk about taking longer walks, having meetings without interruption, and—most telling of all—sitting without hesitation. It was like “finally getting a new chair after years of one with a nail sticking out,” according to one teacher.
Clinics are now greatly simplifying the recuperation process by utilizing improved surgical techniques and developing surgical instruments. Improved patient experiences have been a result of customized post-operative care plans, fiber-focused meal planning, and pain management techniques. Success rates have stayed high over the last ten years, but there have been significantly fewer reports of complications. The entire patient journey has changed, not just the surgery.
Even though preparation is simple, it still needs focus. Before the procedure, patients might be asked to stop taking some blood thinners and fast. A common procedure that increases visibility during surgery and reduces the risk of infection is to empty the bowel using an enema or laxative. Patients who adhere to these procedures frequently recover much more quickly.
A lot of people return home the same day as their procedure. However, since driving is not allowed right after general anesthesia, it is crucial to make transportation arrangements in advance. There may be some weariness during the first few days, as well as some nausea from the anesthetics. Generally speaking, one to two weeks off from work is advised, though more sedentary jobs might allow for an earlier return with caution.
Most testimonies highlight the sense of regaining personal agency as much as the physical improvement. More than just anatomy, hemorrhoids influence behavior, restrict physical activity, and frequently carry emotional burdens. Patients frequently speak of a sort of silent victory when they decide to have surgery. They have addressed a topic that is rarely discussed and have discovered a very dependable solution that has allowed them to proceed.
Haemorrhoidectomy is slowly coming out of the shadows as people’s awareness of digestive health grows. The subject is becoming less taboo thanks to public discourse, online forums, and even late-night comedy segments. It’s easy to find people sharing their post-op experiences on YouTube health channels or Reddit threads. These stories are very valuable, very personal, and frequently funny.
From a wider angle, the tendency toward early surgical intervention points to a change in the priorities of healthcare. Encouraged by better results and compassionate care, people are now seeking long-term solutions earlier rather than enduring discomfort for years. Additionally, medical professionals are becoming more proactive and are now offering this surgery as a logical, progressive option rather than as a last resort.
Although the cost varies by nation and insurance plan, the investment, which is frequently viewed as a significant upfront cost, is recouped in the form of an enhanced quality of life. The process avoids time lost due to physical limitations, incessant prescriptions, and repeated doctor visits. Given its durability, it’s surprisingly inexpensive when looking at cost-effectiveness.




